Infectious Diseases Case of the Month Case #22 |
|||
 |
Two brothers from Michigan, ages 50 and 55, developed fevers, headache, myalgias, and skin lesions after big game hunting in South Africa. The brothers had traveled from Traverse City to South Africa in mid-May and returned twelve days later. While there they engaged in five day guided big game hunts at two locations, one hunt originating from a "camp" north of Johannesburg and the second near Harrismith to the southeast of Johannesburg. The accommodations were relatively luxurious, and food and beverages were supplied by their hosts. Mosquito netting was not used at night. Prior to travel the brothers had received appropriate travel related immunizations and were prescribed atovaquone/proguanil for malaria prophylaxis. Hunting required traveling through thick underbrush. The hunts were quite successful as the brothers succeeded in killing game including eland, impala, gemsbok, wildebeest, hartebeest and others. Carcases of the animals were often noted to be loaded with ticks, and the brothers noted at least one of their guides had what appeared to be numerous insect bites. Neither brother was aware of any insect bites on themselves, and they stopped taking malarial prophylaxis within a day or two of arrival in the first camp as the weather was cool, they saw no mosquitoes, and their guides indicated there was minimal risk. Both brothers, generally in good health, began to feel ill on their airplane flight back to the United States (11 days after first arriving in South Africa). Both experienced malaise and a sense of warmth. Over the next few days both developed waxing and waning fevers to 101o accompanied by myalgias and occasional chills. One brother developed significant headache, the other a cough, and both developed skin lesions. Pictured at left are sores noted on one of the two men. In both cases pictured there was associated with the sores painful regional lympadenopathy (epitrochlear related to the elbow, inguinal to the leg). They also had sparsely distributed papular rashes involving the extremities and torsos (see upper photo). Although the patients appeared moderately ill, their examinations were essentially normal except for the skin findings and the adenopathy. CBCs and comprehensive metabolic panels were normal except one of the two brothers had a very modest thrombocytopenia (plts 134). |
||
What was the likely cause of these brothers' illness? |
|||
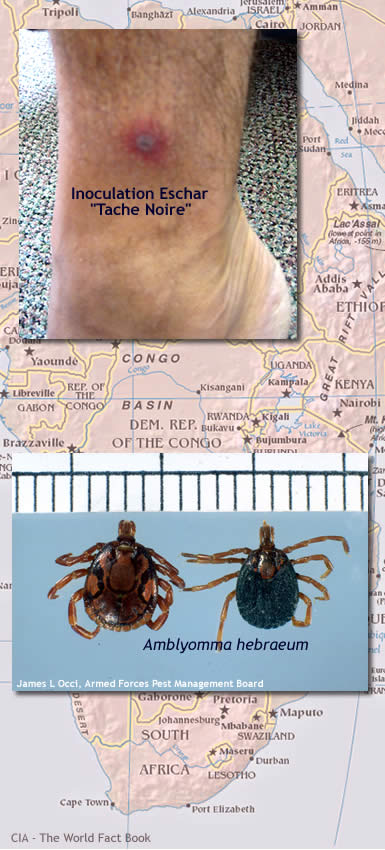 |
These brother big game hunters likely had African Tick Bite Fever cause by Rickettsia africae. The most widespread pathogen responsible for spotted fever in sub-Saharan Africa is Rickettsia africae transmitted by the ticks Amblyomma habraeum and Amblyomma variegatum. A. habraeum (pictured at lower left) is the principle vector in South Africa where the brothers were hunting. Rates of R. africae infection in these ticks are frequently high sometimes exceeding 70%. In contrast to most other hard ticks of medical importance, ticks of the genus Amblyomma actively converge on nearby hosts and behave very aggressively. A single host animal may be attacked by many ticks, and several hosts may be attacked simultaneously. The number of international travel-associated cases of African tick bite fever (ATBF) has increased significantly in recent years. Typically, more than 80% of infected travelers acquire the disease in South Africa where many popular wildlife venues are highly endemic for R. africae infection and where tourism has increased dramatically since the abolition of apartheid. As occurred to the brothers here, cases of ATBF frequently occur in clusters. Game hunting which involves heavy exposure to ground vegetation and ungulates and their hides is an independent risk factor for ATBF. Clinical illness develops usually 5-7 days after bite of an infected tick. Illness is characterized by abrupt onset of flu-like symptoms including fever, fatigue, headache, and myalgias. An inoculation eschar, a black crust surrounded by a red halo (see photo at left), is present in most cases. Multiple eschars, as occurred in the case described, are frequent and are pathognomonic of infection with R. africae reflecting the aggressive behavior of the tick vectors. Regional lymphadenitis is common, and a generalized rash may be present though it tends to occur less commonly and be less prominent than that which occurs in infection with other rickettsia of the spotted fever group. Illness tends to be relatively benign without serious complications or sequelae. Definitive diagnosis is somewhat difficult and unlikely to be available in a timely fashion. R africae antigen can be detected in inoculation eschar biopsies by PCR or immunohistochemistry. Serologies designed to detect R. rickettsii or R. conorii may detect cross reacting antibodies to R africae and thus can be useful. Doxycycline is generally considered effective therapy and perhaps the drug of choice. The brothers in this case were treated with this drug and felt better in 48-72 hours. Francisella tularensis also can cause illness with an inoculation eschar but tularemia does not occur in Africa. MRSA is more apt to cause purulent skin lesions but certainly could at first appear to be an "insect bite." Bacillus anthracis also causes skin lesions that might initially be difficult to distinguish from the eschars of R africae. Untreated illness could be much more severe. Plasmodium falciparum always must be considered in an ill traveler from this region but would not be characterized by inoculation eschars and lymphadenits.
|
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||